What Is Haemoglobin and Why Does It Matter?
Haemoglobin is a protein inside your red blood cells. Its main job is to carry oxygen from your lungs to the rest of your body. When haemoglobin levels are healthy, your cells get the oxygen they need to function efficiently. You feel more energetic, your brain works better, your muscles recover faster, and your body maintains healthy immunity.
When haemoglobin levels drop, oxygen delivery drops too. This is why low haemoglobin levels can make everyday activities like walking, climbing stairs, working, or even getting out of bed feel harder than usual. Many people with low haemoglobin simply feel "off" for weeks or months without understanding the real cause behind their symptoms.
Your blood becomes healthier and performs better when haemoglobin levels stay within the normal range. Let's look at what "normal" means.
Normal Haemoglobin Levels: Understanding What's Healthy
Haemoglobin levels vary by age, gender, and life stage. Normal haemoglobin levels help assess whether your body is getting enough oxygen, whether your red blood cell count is stable, and whether your blood health needs more attention.
Haemoglobin Levels Chart (Age-wise Normal Ranges)
|
Group |
Healthy Haemoglobin Range |
|
Adult Men |
13 - 17 g/dL |
|
Adult Women |
12 - 15.5 g/dL |
|
Pregnancy |
11 - 14 g/dL |
|
Children |
11 - 15.5 g/dL |
These values give a quick snapshot of normal haemoglobin levels, but keep in mind that ranges can vary slightly depending on the lab and individual health.
Haemoglobin Levels in Female: Why Women Are More Vulnerable
Women face unique challenges that make maintaining healthy haemoglobin levels more difficult than for men. This is because the average adult female loses blood every month during menstruation, which affects haemoglobin levels over time. For many women, normal haemoglobin levels by age in females start falling in the teenage years, continue to shift through adulthood, and drop again after childbirth due to postpartum blood loss.

Why Women Are More Vulnerable:
1. Monthly Menstruation
Every month, women lose blood through menstruation. Light periods may cause minimal iron loss, but moderate to heavy periods can deplete iron stores significantly. Women lose approximately 1-3mg of iron daily during their period. Over time, this adds up without proper dietary compensation.
Heavy menstrual bleeding, medically called menorrhagia, affects about 27% of women of reproductive age. If you need to change pads or tampons every 1-2 hours, pass large clots, or have periods lasting more than 7 days, you're at high risk for low haemoglobin.
2. Pregnancy and Childbirth
Pregnancy dramatically increases iron requirements. Your body needs to produce 50% more blood to support the growing baby. The placenta and developing fetus need iron for their own haemoglobin production. This is why prenatal vitamins always contain iron.
During childbirth, women lose blood, further depleting iron stores. Breastfeeding continues to demand extra nutrients. Many women enter their next pregnancy still recovering from iron loss from the previous one, creating a cycle of deficiency.
3. Lower Muscle Mass
Men naturally have more muscle mass than women, and muscle tissue stores myoglobin, an iron-containing protein. This gives men a natural iron reserve that women don't have to the same extent.
4. Dietary Patterns
Many Indian women eat less meat, fish, and eggs due to cultural practices, religious beliefs, or household economics. They often serve food to family members first and eat last, sometimes consuming smaller portions or leftovers with lower nutritional value.
5. Body Weight and Dieting
Women are more likely to follow restrictive diets for weight management. These diets often cut out iron-rich foods or reduce overall calorie intake to levels that don't support adequate nutrition.
Haemoglobin Levels in Pregnancy: Special Considerations
Pregnancy creates unique haemoglobin challenges that every expecting mother should understand.

Why Levels Drop During Pregnancy
Your blood volume increases by approximately 50% during pregnancy to support the baby's development. However, the liquid portion of blood (plasma) increases more than red blood cells, creating a dilution effect. This is called physiological anaemia and is actually normal.
The growing baby needs iron to develop its own blood supply. The placenta requires iron. Your expanding uterus needs increased blood flow. All these demands come from your body's iron stores.
Trimester-Specific Ranges
- First Trimester (Weeks 1-12): Acceptable range is 11.0-14.0 g/dL. Morning sickness often reduces food intake, making adequate iron consumption challenging.
- Second Trimester (Weeks 13-28): Levels of 10.5-13.5 g/dL are considered normal. Blood volume expansion peaks during this period, creating maximum iron demands.
- Third Trimester (Weeks 29-40): Healthy range remains 11.0-13.0 g/dL. The baby builds iron stores for the first 4-6 months of life, drawing heavily from maternal reserves.
Risks of Low Haemoglobin During Pregnancy
Anaemia during pregnancy increases the risk of premature delivery before 37 weeks. Babies may have low birth weight, affecting their health outcomes. Maternal anaemia increases risks during labour and delivery. Post-delivery recovery takes longer. You may experience severe fatigue affecting your ability to care for your newborn. Postpartum depression risk increases with anaemia.
Managing Haemoglobin During Pregnancy
Take prenatal vitamins starting before conception if possible. Eat iron-rich foods at every meal-lean meat, chicken, fish, eggs, leafy greens, legumes, and fortified cereals. Pair plant-based iron with vitamin C foods like citrus fruits, tomatoes, and bell peppers. Avoid tea and coffee, especially near mealtimes. Get tested regularly-at your first prenatal visit, again in the second trimester, and once in the third trimester.
If your doctor prescribes iron supplements, take them consistently. Many pregnant women need 60-120mg of elemental iron daily, much more than the diet can provide.
How to Increase Haemoglobin Levels in Females
Women need additional strategies beyond general recommendations:
-
During Menstruation: Increase iron intake significantly during and immediately after periods when blood loss is highest. Consider short-term supplementation during heavy flow weeks.
-
For Heavy Periods: Track menstrual patterns. If soaking through pads every 1-2 hours or periods lasting over 7 days, consult a gynaecologist. Medical treatment reducing blood loss is as important as increasing iron intake.
-
Pregnancy Planning: Build iron stores 3-6 months before conception. Start prenatal vitamins early. Get baseline haemoglobin testing.
-
Vegetarian Women Face the highest risk, combining low iron absorption from plant foods with monthly blood loss. Consume 1.8 times more iron than non-vegetarians. Never eat iron-rich meals without vitamin C. Include B12 supplements.
Post-Pregnancy: Continue iron-rich foods and supplements for 6+ months after delivery. Breastfeeding increases nutritional demands.
Other than food, women can also improve their haemoglobin through:
- Better sleep routine
- Stress control
- Spacing tea/coffee away from meals
- Managing heavy periods with medical support
- Using iron cookware
- Regular blood tests, especially during menstruation or postpartum
Women's haemoglobin levels are more dynamic because their body goes through many hormonal and physiological changes. Paying attention to these patterns helps maintain a healthy balance.
Haemoglobin Levels in Males: Different Challenges, Different Indicators
Men typically maintain higher haemoglobin levels than women, with normal ranges for adult males falling between 13.5-17.5 g/dL. This biological advantage comes from several factors.
Why Haemoglobin Levels in Males Are Higher
- Testosterone Effect: This hormone stimulates red blood cell production, naturally elevating haemoglobin levels throughout male adulthood.
- Greater Muscle Mass: More muscle tissue provides additional storage for myoglobin, an iron-containing protein.
- No Monthly Blood Loss: Unlike women, men don't experience regular blood loss, allowing them to maintain stable iron stores more easily.
- Typical Dietary Patterns: Men generally consume more protein and meat, providing readily absorbable heme iron.
When Men Develop Low Haemoglobin
Despite these advantages, men can develop low haemoglobin through poor dietary habits (excessive fast food, limited home cooking), intense athletic training that depletes iron stores, internal bleeding from ulcers or gastrointestinal issues, chronic diseases like kidney disorders or thyroid problems, and avoiding routine medical checkups that could detect declining levels early.
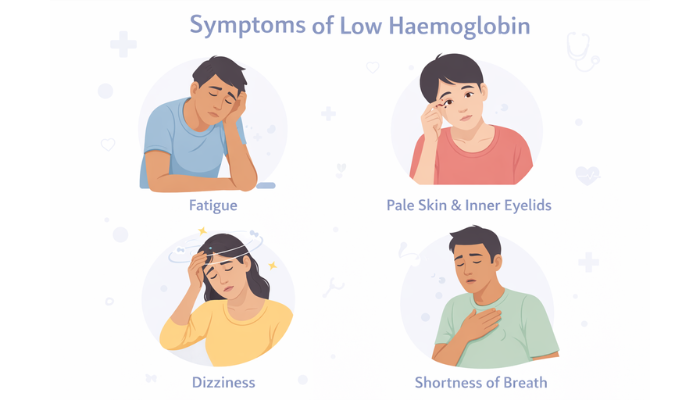
Recognizing Low Hemoglobin Levels: Symptoms and Warning Signs
When haemoglobin levels drop below normal ranges, your body sends clear warning signals. Recognising these symptoms early prevents serious complications.
Symptom Severity by Haemoglobin Level
Mild Anaemia (Haemoglobin 10.0-11.9 g/dL for women, 10.0-13.4 g/dL for men):
- Mild fatigue and tiredness
- Occasional breathlessness with exertion
- Slight difficulty concentrating
- Pale inner eyelids
Moderate Anaemia (Haemoglobin 8.0-9.9 g/dL):
- Constant tiredness despite adequate rest
- Visibly pale skin and nail beds
- Cold hands and feet
- Brittle nails that break easily
- Poor focus and irritability
- Headaches and dizziness
Severe Anaemia (Haemoglobin 6.5-7.9 g/dL):
- Severe weakness limiting daily activities
- Rapid heartbeat even at rest
- Chest discomfort or pressure
- Shortness of breath at rest
- Confusion and memory problems
- Difficulty making decisions
These haemoglobin levels progressively worsen as levels decline, making early detection and treatment crucial.
Dangerously Low Haemoglobin Levels: When to Seek Emergency Care
There's a difference between mildly low haemoglobin and dangerously low haemoglobin levels. When levels fall below 7 g/dL, oxygen supply drops severely and immediate medical attention is needed.
Warning signs of dangerously low levels:
- Breathlessness even while resting
- Chest discomfort
- Very rapid heartbeat
- Fainting or confusion
- Extremely pale or grey skin
- Severe dizziness
- Weakness so intense you can't stand
Pregnant women, older adults, and people with chronic conditions are at higher risk. Emergencies may require iron infusion, oxygen support, or a blood transfusion, depending on severity.
Medical Interventions for Dangerously Low Levels:
- Blood Transfusions: Reserved for haemoglobin below 7 g/dL or severe symptoms. Donor blood directly replaces deficient red blood cells, providing immediate relief within hours.
- IV Iron Infusions: For haemoglobin between 7-9 g/dL when oral supplements won't work fast enough. Iron goes directly into the bloodstream, bypassing the digestive system. Improvement typically occurs within days to weeks.
- Hospitalisation: Severe cases require medical monitoring, especially if heart complications, confusion, or pregnancy complications are present.
At dangerously low haemoglobin levels, even the best diet won't raise levels fast enough, and medical intervention becomes critical and potentially life-saving.
Lifestyle Changes That Support Healthy Haemoglobin
Nutrition is crucial, but other lifestyle factors also affect your blood health.
Exercise Guidelines
- What Helps: Moderate exercise stimulates red blood cell production. Walking 30-45 minutes daily, yoga (especially inversions), swimming, and light cycling all support healthy haemoglobin production.
- What to Avoid: During low haemoglobin, avoid high-intensity interval training, heavy weightlifting, and marathon training. Resume gradually as levels normalise.
Sleep and Recovery
Poor sleep disrupts hormone regulation, controlling red blood cell production. Aim for 7-9 hours nightly, maintain consistent sleep-wake times, and create a dark, cool sleeping environment.
Stress Management
Chronic stress affects nutrient absorption and increases inflammation. Practice daily deep breathing (10-15 minutes), meditation, and maintain a work-life balance.
Other Factors
- Quit smoking: Damages red blood cells and impairs oxygen-carrying capacity.
- Stay hydrated: Drink 8-10 glasses of water daily to support blood volume and circulation.
Monitoring Progress and Knowing When You're Better
Haemoglobin takes time to improve. Most people notice improvement within 3 to 6 weeks, depending on the cause and consistency of treatment.
Signs you're improving:
- Better energy
- Reduced breathlessness
- Improved concentration
- Less dizziness
- Stronger hair and nails
- Higher exercise stamina
You may need follow-up tests every few weeks if your levels were significantly low, if you're pregnant, or if you have an underlying condition.
Conclusion: Why Monitoring Haemoglobin Matters for Your Long-Term Health
Healthy haemoglobin levels are essential for keeping your body energised, your brain sharp, and your organs well-oxygenated. When levels drop, even simple daily activities can start to feel exhausting and because the symptoms often build gradually, many people don’t realise what’s happening until the deficiency becomes severe. Women, especially during menstruation, pregnancy, and postpartum, face an even higher risk and should be particularly mindful of regular testing and nutrition.
The good news? With the right diet, lifestyle habits, medical guidance, and timely monitoring, haemoglobin levels can usually be restored and maintained within a healthy range. If you notice persistent fatigue, breathlessness, weakness, or any warning signs mentioned above, don’t ignore them, speak to your doctor and get your haemoglobin checked. Prioritising your blood health today helps protect your immunity, stamina, and overall wellbeing for years to come.